 I have a bit of a personal interest in Rheumatoid Arthritis (RA). I never knew my grandfather on my mother’s side. In fact, my mother never knew her father (my grandfather). He died from Rheumatoid Arthritis when she was not yet two. He was only 29 and left my grandmother as a single mom to look after three girls, just as the Great Depression began. She managed to get a job and, with the help of close family members, they survived. I respect my grandmother’s achievements as a strong willed independent woman at a time when women generally were not in the workforce. But I know she would have preferred to play the role of housewife and mother with her husband by her side.
I have a bit of a personal interest in Rheumatoid Arthritis (RA). I never knew my grandfather on my mother’s side. In fact, my mother never knew her father (my grandfather). He died from Rheumatoid Arthritis when she was not yet two. He was only 29 and left my grandmother as a single mom to look after three girls, just as the Great Depression began. She managed to get a job and, with the help of close family members, they survived. I respect my grandmother’s achievements as a strong willed independent woman at a time when women generally were not in the workforce. But I know she would have preferred to play the role of housewife and mother with her husband by her side.
My grandfather Ben died a slow and excruciatingly painful death over several years. Toward the end he was curled up in a ball because all of his muscles were perpetually contracted. His hands were described as curled into the shape of claws. Every part of his body was experiencing the pain of torture non-stop. The doctors had no understanding of the disease and no way to treat it other than prescribing strong pain killers. I believe narcotic drugs were the only thing that dulled the pain somewhat.
In my opinion his occupation probably led to his death. My grandfather was a projectionist at the local motion picture theatre. The projection booth, where he spent many hours a day six days a week, was small and not well ventilated. The film of the time was celluloid based, composed of nitrocellulose and camphor. Camphor is a poison that can undergo sublimation at room temperature. The nitrocellulose is extremely flammable and with exposure to heat the nitrate groups can break off and expose nitrogen gases, such as nitrous oxide and nitric oxide. The movie projectors at the time used high temperature light sources. So in the contained environment of the projection booth, with relatively high temperatures, there was likely a high concentration of various toxins.
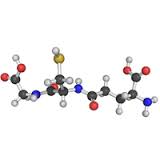
Based on my understanding of the pathology of RA, oxidative stress (high levels of free radicals without adequate levels of antioxidants to neutralize them) is associated with Rheumatoid Arthritis. Given that he worked in a highly toxic environment, the body’s master antioxidant glutathione would have been depleted while trying to remove the toxins from his body. The remaining high levels of free radicals would then go about damaging cells in various parts of the body. In addition, the lack of glutathione would weaken the body’s immune system.
Rheumatoid Arthritis is fairly common in industrialized societies. More women get RA than men. A 2005 study in the United States found that the incidence of RA was about 9.8 women per 1,000; and for men the number was about 4.4 per 1,000. Overall in North America, about 0.6% of the adult population over 18 years of age has Rheumatoid Arthritis. Unfortunately statistics show an increasing trend.
What It Is Not
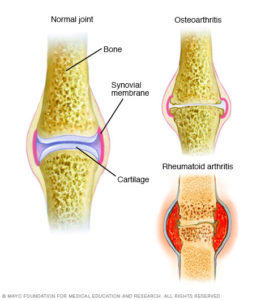
Despite its name, Rheumatoid Arthritis is NOT your grandmother’s Arthritis. When she said her arthritis was acting up, she was most likely referring to the joint pain associated with osteoarthritis.
Rheumatoid Arthritis is a chronic inflammatory disorder that can affect more than just your joints. In some people, the condition also can damage a wide variety of body systems, including the skin, eyes, lungs, heart and blood vessels.
 RA is believed to be an autoimmune disorder. It occurs when your immune system mistakenly attacks your own body’s tissues. That would put in in the same class as Lupus, which is also an autoimmune disorder.
RA is believed to be an autoimmune disorder. It occurs when your immune system mistakenly attacks your own body’s tissues. That would put in in the same class as Lupus, which is also an autoimmune disorder.
Unlike the wear-and-tear damage of osteoarthritis, rheumatoid arthritis affects the lining of your joints, causing a painful swelling that can eventually result in bone erosion and joint deformity.
The reason that RA has “arthritis” in its name is that this term is applied to almost any chronic condition that presents as joint pain.
Possible Causes
When it comes down to it, the medical community says it does not know what causes Rheumatoid Arthritis.
There seems to be some consensus, but no definitive proof, that Rheumatoid Arthritis has as its root certain genetic factors. However, when looking at people with RA and those who do not have the disease, there is no solid linkage. There is simply some statistical correlation between those with RA and those with certain gene markers. The CDC identifies some of the correlations on its web site. This means that there is no solid cause-effect relationship proven. The most that can be said is that certain genetic markers may make a person more prone to developing RA should the triggering mechanism present itself.
Several organizations identify a set of risk factors for RA. The Arthritis Foundation is representative in identifying things like smoking, female hormones, physical or emotional trauma, air pollution, insecticides, and others. It is interesting to note that all of these tend to result in increased levels of free radicals in the body.
Accepted Treatments
Since there is no consensus on the actual cause of RA, the medical community is left with only treating symptoms in an attempt to alleviate pain and slow the progress of the disease.
According to the U.S. Centres for Disease Control (CDC), the contemporary recommended approach to treating RA is very aggressive. Non-biologic disease-modifying antirheumatic drugs (DMARDs), which reduce disease activity and prevent joint deformity, are prescribed within three months of diagnosis. In 2012, the American College of Rheumatology updated RA medical management guidelines. These guidelines describe which biologic DMARDs to use for specific RA disease profiles (e.g., features such as disease activity, signs and symptoms, and prognosis).
Options to Consider
Research paper after research paper confirms that Rheumatoid Arthritis is associated with oxidative stress. There is a 100% correlation. To confirm this, go to PubMed and search for ‘rheumatoid arthritis glutathione’ and you will be presented with a list of hundreds of published papers. Each one will identify low levels of glutathione, which correlates to high levels of oxidative stress. Oxidative stress means that the body has more free radicals than it has antioxidants to neutralize them. Free radicals cause harm to the body and produce cellular inflammation.
It is disturbing to note that with all of this research showing that RA patients have high levels of free radicals, no research is being done to determine the effect of dramatically increasing antioxidant levels in the body – particularly levels of the body’s master antioxidant.
I have said before what I believe the reason to be. There is no money in it. Most medical research is funded in some way by the pharmaceutical industry. Research proposals will only be funded if there is some prospect of a patentable medicine being developed as a result. Antioxidants don’t fall into that category. Since disease related charities are highly influenced by medical and pharmaceutical interests, it is unlikely that funding for such research would come from those sources either.
So if you have RA, what can you do in addition to following your doctor’s recommendations? There are a couple of suggestions I would offer.
These suggestions are based on a few facts. If you have Rheumatoid Arthritis your body is experiencing oxidative stress. Prolonged periods of oxidative stress result in your health deteriorating. You could develop a variety of chronic ailments from heart disease to glaucoma to cancer. The only open question is the rate at which your health will deteriorate. If you want to change this reality you need to address the oxidative stress.
- First, pay attention to your diet and lifestyle to look for changes you can make that will reduce the volume of free radicals produced in your body (e.g., quit smoking, eliminate processed meat from your diet, reduce your exposure to environmental toxins).
- Second, increase the levels of antioxidants in your body to deal with the free radical load. Increasing the antioxidants you ingest is a good start; but the most effective way is to increase your body’s production of glutathione in the cells. (Refer to the article Get Rid of the Radicals!)
The medical advances in treating Rheumatoid Arthritis were 80 years too late for my grandfather. Perhaps in the near future we will understand the actual cause of the disease and develop ways to prevent it.
#healthscience #rheumatoidarthritis #glutathione
Great article, thanks for sharing that