Recently I discovered that an online friend had been diagnosed with Age-related Macular Degeneration (AMD). My instant reaction was ‘I have something that I believe will help.’ But I decided to do a little research to be sure I had my facts right.
Recently I discovered that an online friend had been diagnosed with Age-related Macular Degeneration (AMD). My instant reaction was ‘I have something that I believe will help.’ But I decided to do a little research to be sure I had my facts right.
What is AMD?
According to the U.S. National Institutes of Health, “AMD is a common eye condition and a leading cause of vision loss among people age 50 and older. It causes damage to the macula, a small spot near the center of the retina and the part of the eye needed for sharp, central vision, which lets us see objects that are straight ahead.”
AMD is usually first detected with a standard visual acuity test. Other diagnostic tests (e.g., dilated eye exam, Amsler Grid, Fluorescein Angiogram, Optical Coherence Tomography) may be used to confirm the diagnosis and monitor the progress of the condition.
According to the American Macular Degeneration Foundation, there are two general types of AMD, the “dry” and the “wet” variety.
- In the “dry” type of macular degeneration, the deterioration of the retina is associated with the formation of small yellow deposits, known as drusen, under the macula. This phenomenon leads to a thinning and drying out of the macula, causing the macula to lose its function. The amount of central vision loss is directly related to the location and amount of retinal thinning caused by the drusen.
- In the “wet” type of macular degeneration, abnormal blood vessels (known as choroidal neovascularization or CNV) grow under the retina and macula. These new blood vessels may then bleed and leak fluid, causing the macula to bulge or lift up from its normally flat position, thus distorting or destroying central vision. Under these circumstances, vision loss may be rapid and severe.
Apparently there is no known cure for AMD; however there are some treatments that appear to slow its progress, including monthly injections.
Relevance of Oxidative Stress
Research confirms that AMD, as with most chronic diseases, correlates with abnormally low blood glutathione levels – which means the body is experiencing high levels of oxidative stress (Reference 1 and Reference 2). Oxidative stress is a state in which the body has more damaging free radicals than it has the antioxidant capacity to neutralize. High levels of free radicals can do much harm across a variety of the body’s systems, including its visual sensory systems.
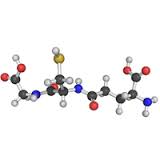
Glutathione (rhymes with ‘glue-da-tie-on’) is a molecule that is produced by every living cell in your body. It is necessary for life in every mammal, including humans. If all of the glutathione were to leave your body, you would not survive two seconds. If you don’t have enough glutathione bad things happen, including disease.
Since glutathione (GSH) is the body’s master antioxidant, a low level of GSH means high oxidative stress. With some exceptions, glutathione is in adequate supply in children. However, from about age 20 onward the natural production of glutathione tends to drop at an average rate of about 10-15 percent per decade. This is a concern because the glutathione molecule is involved in many necessary processes in your body.
In the case of AMD, the “age-related” portion of the name is indicative of the root cause of the condition. The older a person gets the lower their natural intracellular glutathione levels are. AMD is always associated with low glutathione. Therefore it is reasonable to presume that those who are able to keep their intracellular GSH at nominal levels will not develop AMD.
Possible Treatment Option
The natural conclusion this implies is that to slow or stop the progress of the condition in the person who has AMD, they should increase their intracellular glutathione levels substantially. This is a conclusion that was reached in a 2013 study (Reference 3). But as with similar research findings for other chronic diseases, no follow-up work is done to bring this to standard treatment practice. Many folk believe this is because there is no money to be made by the medical and pharmaceutical industries from the use of relatively inexpensive nutritional supplements.
When I heard about my online friend having the “wet” form of AMD, I put a question out to a group of folk that know about glutathione.
Here’s what I asked: Increasing glutathione is supposed to help with macular degeneration. Does anyone know of someone who experienced this effect? I’m unsure what I can tell a friend who I just found out has the condition. Thanks.
After a couple of days, here’s a response I got from a personal friend in the group: Hi John, I have had macular degeneration for many years. My ophthalmologist takes a picture of my left eye every year. It was full of blood spots and lines of blood. Now it is smooth and no blood at all. Big change in about one year. Yeah for <product name>.
The product he named is one that increases intracellular GSH levels. This is one person’s experience. By itself it does not mean this constitutes a confirmed treatment or a cure. But in my mind it is further evidence that the medical community really needs to take a look at increasing intracellular glutathione levels as a bona fide treatment option for chronic diseases like AMD.
References:
Reference 1: Qin L, Mroczkowska SA, Ekart A, Patel SR, Gibson JM, Gherghel D., Patients with early age-related macular degeneration exhibit signs of macro- and micro-vascular disease and abnormal blood glutathione levels, Graefe’s archive for clinical and experimental ophthalmology, (January 2014)
Reference 2: Mrowicka M, Mrowicki J, Szaflik JP, Szaflik MS, Ulińska M, Szaflik J, Majsterek I., Evaluation pro/antioxidant balance in patients with wet form of age-related macular degeneration, Klin Oczna. 2016;118(4):284-8 (original article in Polish)
Reference 3: Zafrilla P, Losada M, Perez A, Caravaca G, Mulero J., Biomarkers of oxidative stress in patients with wet age related macular degeneration, The Journal of Nutrition, Health & Aging. (March 2013)
#amd #chronicdisease #glutathione