 Glutathione (rhymes with ‘glue-da-tie-on’) is a molecule that is produced by every living cell in your body. It is necessary for life in every mammal, including humans. If all of the glutathione were to leave your body, you would not survive two seconds. If you don’t have enough glutathione bad things happen, including disease.
Glutathione (rhymes with ‘glue-da-tie-on’) is a molecule that is produced by every living cell in your body. It is necessary for life in every mammal, including humans. If all of the glutathione were to leave your body, you would not survive two seconds. If you don’t have enough glutathione bad things happen, including disease.
Glutathione (chemical designation GSH) is a protein, specifically a tripeptide. It is composed of three amino acids – glutamic acid, cysteine, and glycine. The cysteine amino acid contains a sulphur group which is responsible for many of the beneficial chemical properties of the whole glutathione protein.
With some exceptions, glutathione is in adequate supply in children. However, from about age 20 onward the natural production of glutathione tends to drop at an average rate of about 10-15 percent per decade. What this means is that when you are in your 40s, 50s, and 60s your natural glutathione production may be about half of what it was when you were a healthy 18 year old. This is a concern because the glutathione molecule is involved in many necessary processes in your body. Only some of them are outlined here.
The Cells of Your Body
It is difficult to get an accurate count. However, there seems to be some consensus that the human body has somewhere between 35 trillion and 70 trillion cells (excluding bacteria), depending on the size of the body and other factors.
Each cell has a role or mission. That mission is programmed by its DNA. The cells have different lifespans. For example red blood cells have a lifespan of about 120 days; whereas the lifespan of a white blood cell is much shorter. The average is about 90 days. What this means is that about every three months your body has completely replaced itself. Before a cell dies, it initiates the creation of its successor. And that successor is an exact duplicate of itself, including any damage or faults it may have. The body produces about 40 billion new cells every day!
Generating Energy in the Cell
In order for a cell to fulfill its mission and do its work it needs motion. The motion is provided by the cell’s mitochondria. You can think of the mitochondria as a tiny motor. Cells have many mitochondria. The number depends on the cell’s mission or type. For example, a fat cell typically has only a couple of mitochondria; whereas a heart cell has about 2,500 mitochondria.
The mitochondria need fuel. That fuel is Adenosine Triphosphate (ATP). Glutathione is part of the process of generating ATP. When glutathione levels are down, the production of ATP slows and a person experiences low energy levels. ATP is needed for muscle contraction, so athletes are particularly concerned about their levels of ATP. Raising glutathione levels can enhance athletic performance.
Neutralizing Free Radicals
When the fuel (ATP) is used to generate energy for the mitochondria to initiate the work of the cell, it produces waste products (that you can think of as exhaust from the motor) called free radicals. Free radicals are dangerous because, with their unbalanced electrical charge, they initiate a chemical reaction with almost any molecule in the cell that they come in contact with. This causes damage to the cell.
In addition, when the cell encounters toxic substances and tries to deal with the toxins, free radicals are produced in alarming numbers.
Glutathione neutralizes the harmful free radical by neutralizing the unbalanced charge on the radical molecule. In fact, glutathione is the body’s primary antioxidant. Adequate levels of glutathione protect the cell by neutralizing the free radicals. However, if there are inadequate amounts of glutathione, the remaining free radicals will do more and more damage.
Oxidative stress is defined as a state where the free radical load on the body exceeds the antioxidant capacity of the body. Prolonged periods of oxidative stress can be shown to result in chronic diseases of various sorts. (Refer to Diseases and Conditions Associated with Oxidative Stress.) There is good reason to want to maintain adequate glutathione levels.
Recycling Antioxidants
Glutathione (GSH) as an antioxidant is able to recycle itself. After neutralizing the free radical by dealing with its negative charge, it combines with another glutathione molecule to form an electrically neutral GSSH molecule that is subsequently transformed back into a GSH molecule.
There are only a few antioxidants that can be recycled (e.g., Vitamin E, Vitamin C, alpha lipoic acid (ALA) and Glutathione). Vitamin E, Vitamin C and ALA are recycled by GSH. So low glutathione levels limit the ability of these other antioxidants to do their job. GSH on the other hand can recycle itself many thousands of times.
Therefore the effectiveness of certain of the antioxidants you ingest and the overall antioxidant capacity of your body is limited by the availability of glutathione.
Synthesizing Antioxidants and Proteins
Each antioxidant must be synthesized into a useable state before it can be used by the cells. The primary synthesizing agent for antioxidants is glutathione.
Proteins must also be synthesized before they can be used by the cells. Glutathione is not the sole synthesizing agent for proteins – but it is a principal agent. So the level of glutathione in the cell is a major factor in the degree to which ingested proteins can be used by the body.
Reducing Cellular Inflammation
For several decades there has been a mounting belief in the medical research community that cellular inflammation is the root cause of virtually all chronic disease. However, in my research I have been unable to unearth the direct cause-effect relationship between inflammation and disease.
What I do know is that cellular inflammation seems to go hand in hand with oxidative stress. It would appear that when the huge volume of free radicals do damage to the cells during periods of oxidative stress, the reaction of the cell to this insult is to become inflamed. If this is the case, the cause of chronic disease is prolonged periods of oxidative stress – and cellular inflammation is just a resulting symptom.
Regardless of the exact mechanism, what we do know with some certainty is that in the presence of abundant glutathione the level of cellular inflammation goes down.
Detoxifying Heavy Metals and Environmental Toxins
Many heavy metals like lead and mercury are toxic to the body and can cause devastating damage. For over a hundred years these substances have been used in a variety industrial processes. Lead was used in oil based paint and in gasoline. It was only after significant portions of the population started to have obvious disease symptoms that laws were passed to reduce or eliminate such use.
Regardless, these substances are still working their way through the environment. For example, mercury has found its way into the food chain and has been detected in disconcerting concentrations in fish like tuna. That is why there are warnings about limiting the amount of tuna you include in your diet.
Sometimes heavy metal molecules get sequestered in fat cells where they do little harm. But when you lose weight they are released to circulate and possibly find a home in other cells where they can do damage. At other times the heavy metals you ingest go directly to cells where they could do harm.
If you have adequate levels of glutathione, the GSH molecule will interact with the heavy metal molecule and escort it out of your system. This is where the sulphur group on the cysteine part of GSH comes into play. Sulphur is ‘sticky’ and this is how the GHS molecule attaches to the heavy metal molecule. The combined compound then gets flushed out of your system. (Drink lots of water to facilitate this detoxification process.) This process is called chelation.
In addition, there are innumerable environmental toxins that are not metals that our bodies encounter. The list includes petroleum byproducts, pesticides, prescription drugs, cleaning compounds, alcohol, and on and on. The glutathione molecule is instrumental in removing these various toxins from the cell and facilitates their removal from the body. It does so by breaking down the fat soluble toxin, attaching itself to the toxin fragments thus making them water soluble, and then as a water soluble compound it can be flushed out of the system through the kidneys.
In fact there is an organ that has as its primary function toxic chemical detoxification. The liver has been referred to as the body’s “washing machine” because it extracts toxins from the blood flow and removes them to be eliminated through excretion. Glutathione is critical to this chemical process. It is not surprising, therefore, that the liver has the highest concentration of glutathione in the body. Adequate levels of glutathione in the liver are essential to ongoing good health.
Unfortunately this activity depletes glutathione levels, leaving less glutathione to generate energy for the cell to do its work and less glutathione to neutralize free radicals. Furthermore, the load of environmental toxins is increasing every year.
Protecting Mitochondrial DNA
It is believed that the effects of aging are a result of repeated minor damage to cellular mitochondrial DNA over time. When a cell with damaged DNA reproduces, the resulting cell may not function as well as the original cell prior to the damage. After a while the effect accumulates and you start to notice the typical characteristics of aging. Furthermore, some DNA damage is not minor and instead of gradual aging we see a specific disease condition become apparent. (One example of this is the DNA damage that causes tumorous growth.)
There are three primary causes of DNA damage:
- heavy metals
- chemical toxins
- radiation
In the case of heavy metals, we have seen that abundant glutathione can chelate the metal, removing these molecules from the cell and from your body. This removes the opportunity to damage the DNA.
Likewise in the case of chemical toxins, abundant glutathione facilitates the removal of these harmful molecules from the cell and from the body, primarily through the liver.
High levels of glutathione also protect mitochondrial DNA from radiation damage.
We are exposed to radiation in a variety of ways. There is diagnostic imaging (think x-rays), radiation therapy (a standard cancer treatment), background radiation (think UV radiation that causes sun tans), cosmic radiation and other types.
I don’t know what the exact number is, but I have been given to understand that the level of damaging radiation is at least 1,000 times greater at a height of 30,000 metres than at sea level. This is of concern to commercial air crew who typically fly many hours a day at more than 10,000 metres, and to astronauts who operate much higher than 30 kilometres above the earth.
A study published in 2000 and funded jointly by the National Aeronautics and Space Administration (NASA), NASA Goddard Space Flight Center, the National Institutes of Health, and the U.S. Department of Energy found that significantly increasing glutathione levels would be very beneficial for “reducing the load of mutations created by high LET radiation in astronauts or other exposed individuals.” Of interest is the fact that cancer radiation therapy also uses high LET radiation.
So astronauts, commercial air crew members, and anyone undergoing radiation therapy should have a particular interest in increasing their body’s glutathione levels.
Facilitating Hemoglobin Function
Hemoglobin is the active component of red blood cells that carries oxygen from the lungs to the cells throughout the body. Glutathione reduces hemoglobin to a +2 state so it can accept oxygen and carry it to the cells. Low glutathione levels could reduce the level of oxygen that gets to the cells, which in turn could lead to a wide range of adverse consequences.
Abundant glutathione levels tend to bring hemoglobin counts into the normal range.
Optimizing the Immune System
The immune system is complex. A couple of primary components are the white blood cells (leukocytes) which are key to tackling bacterial and viral infections, and the natural killer cells (like the Killer T cells) that destroy compromised host cells, such as tumor cells or virus-infected cells.
With low glutathione levels, the immune system will respond sluggishly. There is considerable evidence that glutathione plays a key role in the regulation and control mechanisms of the immune response to a threat.
Abundant levels of glutathione allow the immune system to respond explosively to a bacterial or viral insult. High GSH levels result in an optimized immune system.
Enhancing Wound Healing
Have you ever noticed that when children get a minor cut or scrape they heal very quickly as compared with their parents or grandparents? And their scarring is much less as well.
It looks like glutathione is responsible.
A study was completed in 2014 and the peer reviewed result was published in 2015. It clearly showed that raising glutathione levels before surgery (a surgical incision is considered a wound in medicine) and keeping them elevated after surgery dramatically reduced the healing time, increased the strength of the healed wound, and significantly reduced any resulting scar.
The belief is that these results are brought on by a substantial reduction of inflammation around the site of the wound.
So if you are facing surgery, increase your glutathione levels substantially at least for the period two or more weeks before the surgery and two to four weeks (or more) afterward.
Reducing “Bad Cholesterol”
Low density lipoproteins (LDL) are considered to be the “bad cholesterol.” According to the American Heart Association:
LDL cholesterol is considered the “bad” cholesterol because it contributes to plaque, a thick, hard deposit that can clog arteries and make them less flexible. This condition is known as atherosclerosis. If a clot forms and blocks a narrowed artery, heart attack or stroke can result. Another condition called peripheral artery disease can develop when plaque buildup narrows an artery supplying blood to the legs.
For years there has been widespread anecdotal evidence that high glutathione levels were associated with reduced blood serum LDL.
A study to look at this was completed in late 2014 and the peer reviewed result was published in 2016. It concluded that elevated glutathione levels resulted in “significant decreases in LDL.” It lowers LDL, Lp(a) and oxidised lipid concentrations.
Summary
Glutathione is a key participant in a wide variety of the body’s processes. It is absolutely essential to good health. Diminished glutathione levels can have adverse effects that may manifest in many different ways, sometimes displaying several such manifestations at the same time.
Increasing glutathione to optimum levels in the body is vital to maintaining good health over time.
p.s. To find out what I use personally to elevate glutathione levels, go to the Contact John menu item and send me a message.
#glutathione #healthscience #chronicdisease
 Recently I discovered that an online friend had been diagnosed with Age-related Macular Degeneration (AMD). My instant reaction was ‘I have something that I believe will help.’ But I decided to do a little research to be sure I had my facts right.
Recently I discovered that an online friend had been diagnosed with Age-related Macular Degeneration (AMD). My instant reaction was ‘I have something that I believe will help.’ But I decided to do a little research to be sure I had my facts right.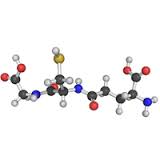
 This is a topic that is somewhat dear to my heart. My sister was diagnosed with Fibromyalgia a couple of decades ago. And her life has been miserable for much of that time.
This is a topic that is somewhat dear to my heart. My sister was diagnosed with Fibromyalgia a couple of decades ago. And her life has been miserable for much of that time.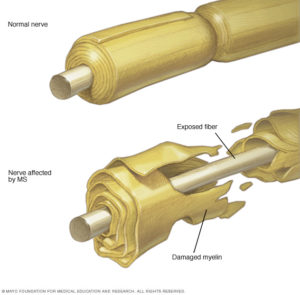 According to the Mayo Clinic, “Multiple sclerosis (MS) is a potentially disabling disease of the brain and spinal cord (central nervous system). In MS, the immune system attacks the protective sheath (myelin) that covers nerve fibers and causes communication problems between your brain and the rest of your body. Eventually, the disease can cause the nerves themselves to deteriorate or become permanently damaged.”
According to the Mayo Clinic, “Multiple sclerosis (MS) is a potentially disabling disease of the brain and spinal cord (central nervous system). In MS, the immune system attacks the protective sheath (myelin) that covers nerve fibers and causes communication problems between your brain and the rest of your body. Eventually, the disease can cause the nerves themselves to deteriorate or become permanently damaged.” I have a bit of a personal interest in Rheumatoid Arthritis (RA). I never knew my grandfather on my mother’s side. In fact, my mother never knew her father (my grandfather). He died from Rheumatoid Arthritis when she was not yet two. He was only 29 and left my grandmother as a single mom to look after three girls, just as the Great Depression began. She managed to get a job and, with the help of close family members, they survived. I respect my grandmother’s achievements as a strong willed independent woman at a time when women generally were not in the workforce. But I know she would have preferred to play the role of housewife and mother with her husband by her side.
I have a bit of a personal interest in Rheumatoid Arthritis (RA). I never knew my grandfather on my mother’s side. In fact, my mother never knew her father (my grandfather). He died from Rheumatoid Arthritis when she was not yet two. He was only 29 and left my grandmother as a single mom to look after three girls, just as the Great Depression began. She managed to get a job and, with the help of close family members, they survived. I respect my grandmother’s achievements as a strong willed independent woman at a time when women generally were not in the workforce. But I know she would have preferred to play the role of housewife and mother with her husband by her side.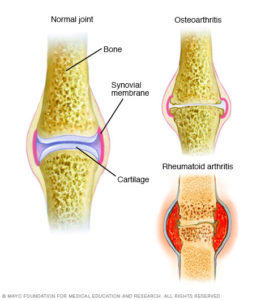 RA is believed to be an autoimmune disorder. It occurs when your immune system mistakenly attacks your own body’s tissues. That would put in in the same class as Lupus, which is also an autoimmune disorder.
RA is believed to be an autoimmune disorder. It occurs when your immune system mistakenly attacks your own body’s tissues. That would put in in the same class as Lupus, which is also an autoimmune disorder. Glutathione (rhymes with ‘glue-da-tie-on’) is a molecule that is produced by every living cell in your body. It is necessary for life in every mammal, including humans. If all of the glutathione were to leave your body, you would not survive two seconds. If you don’t have enough glutathione bad things happen, including disease.
Glutathione (rhymes with ‘glue-da-tie-on’) is a molecule that is produced by every living cell in your body. It is necessary for life in every mammal, including humans. If all of the glutathione were to leave your body, you would not survive two seconds. If you don’t have enough glutathione bad things happen, including disease.