 There are probably more years behind me than in front of me. My analytical approach over that time caused me to observe random things and store them. Then later I would try to make sense of them – how did they fit together? Was there a pattern? One of the things I noticed, and I think epidemiologists would confirm it, is that there seems to have been an increase in the incidence of a variety of physical conditions that did not have as a root cause either bacterial infection or a virus. The pattern seems to have started shortly after World War II, but may have originated earlier. You may have noticed the same trend.
There are probably more years behind me than in front of me. My analytical approach over that time caused me to observe random things and store them. Then later I would try to make sense of them – how did they fit together? Was there a pattern? One of the things I noticed, and I think epidemiologists would confirm it, is that there seems to have been an increase in the incidence of a variety of physical conditions that did not have as a root cause either bacterial infection or a virus. The pattern seems to have started shortly after World War II, but may have originated earlier. You may have noticed the same trend.
The Pattern
When I was growing up in the 50s and 60s, asthma was rare and now it is common among young people. Autism was virtually unheard of and now the incidence seems to be higher than 1 in 100 male births in Western society. Cancer was not as rare, probably because smoking was a standard pastime, cigarettes were unfiltered at the time, and people were dying from lung cancer. But the rate of all different kinds of cancers has climbed dramatically over the past 50 years. The same holds true, to varying degrees, for things like Parkinson’s, Rheumatoid Arthritis, Fibromyalgia, Multiple Sclerosis and most other chronic diseases. What was going on? All of these conditions are quite different from each other; but they were all displaying a similar incidence pattern.
The ‘ah-ha’ Moment
Occasionally I like to do a bit of personal research in the area of science and health. Recently I came across an online article entitled What Is Cancer? And in the body of the article was the heading “Cancer is a symptom not a disease.” That brought me up short. And to be honest, I didn’t finish reading the article. My mind went off in a totally different direction.
Cancer is a symptom, not a disease. If that is true, of what is it a symptom? And could it also be true for those other conditions that were displaying this common incidence trend that I found intellectually irritating? I know that there are over 70 diseases and conditions associated with low glutathione. And all of the conditions displaying the trend are on the list. That commonality could not be a fluke.
Sometimes research involves serendipity. A few days later I saw that Time magazine, on the cover of its February 23, 2004 issue, had proclaimed “The surprising link between INFLAMMATION and HEART ATTACKS, CANCER, ALZHEIMER’S and other diseases.” The article inside said:
“What does a stubbed toe or a splinter in a finger have to do with your risk of developing Alzheimer’s disease, suffering a heart attack or succumbing to colon cancer? More than you might think. As scientists delve deeper into the fundamental causes of those and other illnesses, they are starting to see links to an age-old immunological defense mechanism called inflammation…”
The Mechanism
There seems to be increasing agreement in the medical research community that cellular inflammation is a common cause of most chronic disease in the world. Here’s where things get interesting.
- Most cellular inflammation results from oxidative stress.
- Oxidative stress is caused by an over abundance of free radicals in the cell. In fact it is defined as the condition that occurs when the sum of free radicals in a cell exceeds the antioxidant capacity of the cell.
- Free radicals are produced when the cell does some work. Work can include normal things like breathing, moving, and thinking (depending on the type of cell). The ‘work’ uses oxygen and the result of that process (the exhaust of the oxygen burn if you will) is the production of free radicals. But where things start to go wrong is when the work involved is the cell trying to deal with toxins and other substances that don’t belong in the cell. This activity represents a lot of work and produces huge amounts of free radicals.
- Antioxidants are the compounds that rid the cell of free radicals. If there is an adequate supply of antioxidants in the cell, the level of free radicals can be maintained at a manageable level. However, if the level of free radical production is excessive (e.g. from the work of trying to deal with a buildup of toxins) the cell’s antioxidants are unable maintain a reasonable balance. The level of antioxidants decreases as they are used to get rid of the free radicals. In this situation, the cell works less and less efficiently, oxidative stress increases and, if left unchecked for a significant period of time, disease results.
Glutathione is the body’s master antioxidant. In addition to being an antioxidant in its own right it also facilitates the work of other antioxidants. For example, in the absence of glutathione Vitamin C would be unable to perform as an antioxidant. Glutathione is produced on demand in every living cell in the body. It is also a key component needed for many of the cell’s base functions to work. So if there is not an adequate supply of glutathione in the cell, not only is the cell unable to deal with free radicals but it is also unable to perform its main cellular functions at an optimal level.
Since glutathione is key to ridding the cell of free radicals, most researchers use the level of glutathione in the body as the primary measure of oxidative stress. Low levels of glutathione equals high levels of oxidative stress.
The Key Component
Glutathione is a tripeptide composed of three amino acids. These are glutamic acid, cysteine, and glycine. The cysteine amino acid contains a sulphur group responsible for many of the chemical properties of the whole glutathione protein.
Glutathione is produced on demand in the cell. The level of glutathione produced by the body is normally high during childhood and is at its natural peak at about age 20. The level then diminishes at an average rate of about 1% to 1.5% per year. Production is dependent on the availability of the raw materials – the glutamic acid, cysteine, and glycine. In most people there is an adequate supply of glutamic acid and glycine. The limiting factor is the availability of cysteine with an intact sulphur group. This compound is not normally found in abundant quantities in our diet.
The natural result of all of this is that by the time people reach their 40s and 50s they are starting to feel their age and the incidence of chronic disease increases dramatically. This is not surprising since their glutathione levels are half of what they were at 20. The level of exposure in our modern society to untold numbers of environmental toxins and other stressors makes the situation worse than it might be otherwise. So in recent decades we see the incidence of chronic diseases, that used to be associated with old age, occurring when people are younger and younger.
The Theory
It would seem that increasing intracellular glutathione (glutathione inside the cell, produced by the cell) would go a long way to reducing a variety of chronic diseases.
There are many ways to increase glutathione levels. Some have minimal effect while others increase intracellular glutathione considerably. I take a glutathione enhancing supplement that study results show increases intracellular glutathione levels several times more effectively than the next best method.
So if there is evolving consensus that cellular inflammation is the root cause of cancer and a variety of other chronic conditions, why have there not been studies done on treatment and prevention of these conditions with large amounts of antioxidants, including increasing glutathione levels within the cells?
The Black Hats
Such clinical studies can be expensive. Most of the money for treatment studies has traditionally come, in one form or another, from the pharmaceutical industry. But the pharmaceutical industry is big business, apparently in the Trillion Dollar range. In May of 2015, Forbes published an article with a headline that read “The Cancer Drug Market Just Hit $100 Billion And Could Jump 50% In Four Years”.
 This means that a full 10% of big pharma revenue comes from cancer alone. It is not in the best interests of these companies to fund studies that could result in identification of effective cancer treatments that involve inexpensive natural antioxidants. In fact, it is in their interests to actively prevent that happening. And the committees that make funding decisions in the various disease-focused charities are heavily influenced by the medical and pharmaceutical industries.
This means that a full 10% of big pharma revenue comes from cancer alone. It is not in the best interests of these companies to fund studies that could result in identification of effective cancer treatments that involve inexpensive natural antioxidants. In fact, it is in their interests to actively prevent that happening. And the committees that make funding decisions in the various disease-focused charities are heavily influenced by the medical and pharmaceutical industries.
It is interesting to note that, because most pharmaceutical drugs are toxic poisons, treatments for diseases like chemo for cancer end up making the cellular inflammation worse – for all the cells in the body, not just the lumps and bumps that they are trying to target. Does anybody wonder why when the doctors manage to kill a tumor, some time later in some formerly unaffected part of the body, a “new” cancer pops up? (But the doctor doesn’t tell you that. He says that the cancer spread.)
The Conclusion
There are many documented cases of non-traditional treatments being successful. The common thread that ties most of them together is each has elements that increase the body’s antioxidant levels significantly. These successes should be applauded and explored for broader adoption – not attacked.
Was the information in the Time article followed up at all with further research? Not that I can see. And it would appear that further articles on the same topic in other major publications were actively discouraged. I find the situation frustrating in the extreme! And if my suppositions are true, what is happening is criminal.
Cancer is not a disease. It is a symptom. First and foremost it is a symptom of prolonged periods of oxidative stress in the body. But it is also a symptom of unnaturally high levels of toxins in our environment, a symptom of a pattern that applies to many other diseases, and a symptom of a powerful segment of the business community putting profits ahead of human life.
What is your view? I urge you to leave a comment.
Fact vs. Hypothesis vs. Opinion
It is a fact that all forms of cancer and most other chronic diseases have cellular inflammation as a fundamental characteristic.
To verify this for yourself, you can use Pubmed. Pubmed is the U.S. government site, operated by the National Institutes of Health, that is a global library of published papers on medical science. Go to pubmed.gov and enter the search terms ‘glutathione’ and the name of any disease of interest (e.g., cancer, melanoma, asthma). You will get a (potentially long) list of published papers. Randomly look at the studies and you will see that all of them show low glutathione levels for those subjects with the condition. Virtually any researcher in the field will tell you that this indicates high levels of oxidative stress and consequently high levels of cellular inflammation.
The corollary is also true. If glutathione levels are raised to optimum levels in the cells in the presence of supporting nutrients, free radicals will be eliminated, oxidative stress will be reduced and cellular inflammation will be reduced.
It is my hypothesis that increasing intracellular glutathione levels to nominal levels will reduce the symptoms of the condition in question and possibly prevent the condition from occurring in the first place. This assertion is based on the logic that the body’s natural functions will protect itself if the necessary ‘raw materials’ are available to do the job. Low glutathione levels represent one such lack of ‘raw materials’. By having an optimum level of glutathione and other supporting antioxidants available in the cells, free radical levels will stay in healthy balance, energy will be available to the mitochondria, and the immune system will be able to function as it was designed.
It is my opinion, based on the mountain of evidence found in the Pubmed studies which suggest my hypothesis holds true, that the pharmaceutical industry is actively preventing the conduct of suitable studies to validate the hypothesis. The evidence that links inflammation to disease has been building for decades. I can’t believe I am the only person to have seen the pattern. The 2004 article in Time verifies that I’m not.
Forensic accountants always tell you to “follow the money” to look for motive. Who benefits from this lack of action? Clearly it is the pharmaceutical industry. More than $100 Billion EACH YEAR can buy quite a few votes in various legislative bodies around the world, can buy modified research results, can buy doctors willing to toe the line on what constitutes acceptable medical practice. Thus my opinion. It is a nasty conclusion to reach; but one I think is justified by the available facts.
#cancer #glutathione #chronicdisease #healthscience
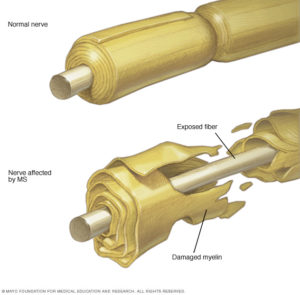 According to the Mayo Clinic, “Multiple sclerosis (MS) is a potentially disabling disease of the brain and spinal cord (central nervous system). In MS, the immune system attacks the protective sheath (myelin) that covers nerve fibers and causes communication problems between your brain and the rest of your body. Eventually, the disease can cause the nerves themselves to deteriorate or become permanently damaged.”
According to the Mayo Clinic, “Multiple sclerosis (MS) is a potentially disabling disease of the brain and spinal cord (central nervous system). In MS, the immune system attacks the protective sheath (myelin) that covers nerve fibers and causes communication problems between your brain and the rest of your body. Eventually, the disease can cause the nerves themselves to deteriorate or become permanently damaged.”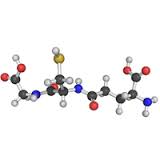
 I have a bit of a personal interest in Rheumatoid Arthritis (RA). I never knew my grandfather on my mother’s side. In fact, my mother never knew her father (my grandfather). He died from Rheumatoid Arthritis when she was not yet two. He was only 29 and left my grandmother as a single mom to look after three girls, just as the Great Depression began. She managed to get a job and, with the help of close family members, they survived. I respect my grandmother’s achievements as a strong willed independent woman at a time when women generally were not in the workforce. But I know she would have preferred to play the role of housewife and mother with her husband by her side.
I have a bit of a personal interest in Rheumatoid Arthritis (RA). I never knew my grandfather on my mother’s side. In fact, my mother never knew her father (my grandfather). He died from Rheumatoid Arthritis when she was not yet two. He was only 29 and left my grandmother as a single mom to look after three girls, just as the Great Depression began. She managed to get a job and, with the help of close family members, they survived. I respect my grandmother’s achievements as a strong willed independent woman at a time when women generally were not in the workforce. But I know she would have preferred to play the role of housewife and mother with her husband by her side.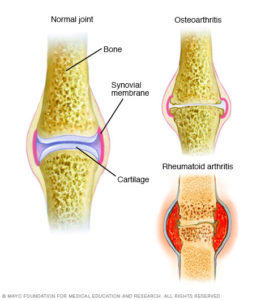 RA is believed to be an autoimmune disorder. It occurs when your immune system mistakenly attacks your own body’s tissues. That would put in in the same class as Lupus, which is also an autoimmune disorder.
RA is believed to be an autoimmune disorder. It occurs when your immune system mistakenly attacks your own body’s tissues. That would put in in the same class as Lupus, which is also an autoimmune disorder.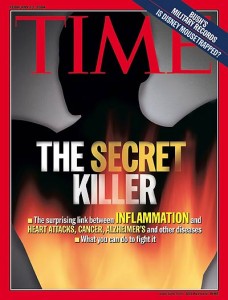 There are probably more years behind me than in front of me. My analytical approach over that time caused me to observe random things and store them. Then later I would try to make sense of them – how did they fit together? Was there a pattern? One of the things I noticed, and I think epidemiologists would confirm it, is that there seems to have been an increase in the incidence of a variety of physical conditions that did not have as a root cause either bacterial infection or a virus. The pattern seems to have started shortly after World War II, but may have originated earlier. You may have noticed the same trend.
There are probably more years behind me than in front of me. My analytical approach over that time caused me to observe random things and store them. Then later I would try to make sense of them – how did they fit together? Was there a pattern? One of the things I noticed, and I think epidemiologists would confirm it, is that there seems to have been an increase in the incidence of a variety of physical conditions that did not have as a root cause either bacterial infection or a virus. The pattern seems to have started shortly after World War II, but may have originated earlier. You may have noticed the same trend. This means that a full 10% of big pharma revenue comes from cancer alone. It is not in the best interests of these companies to fund studies that could result in identification of effective cancer treatments that involve inexpensive natural antioxidants. In fact, it is in their interests to actively prevent that happening. And the committees that make funding decisions in the various disease-focused charities are heavily influenced by the medical and pharmaceutical industries.
This means that a full 10% of big pharma revenue comes from cancer alone. It is not in the best interests of these companies to fund studies that could result in identification of effective cancer treatments that involve inexpensive natural antioxidants. In fact, it is in their interests to actively prevent that happening. And the committees that make funding decisions in the various disease-focused charities are heavily influenced by the medical and pharmaceutical industries. Yesterday I was in the gym change room just getting ready to go home after a workout. A fellow came in after finishing his workout. There was a light clunk when he opened his locker, a few down from mine. On the floor between us was a small bottle, with a protrusion at right angles out the side of the bottle. I asked if that was his puffer.
Yesterday I was in the gym change room just getting ready to go home after a workout. A fellow came in after finishing his workout. There was a light clunk when he opened his locker, a few down from mine. On the floor between us was a small bottle, with a protrusion at right angles out the side of the bottle. I asked if that was his puffer.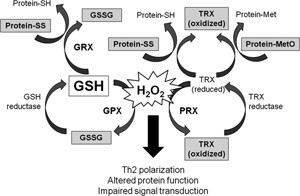 One of the conclusions seemed to be that if there is insufficient glutathione (GSH) available in the cell, the level of free radicals will increase. An imbalance represented by high levels of free radicals results in oxidative stress and cellular inflammation. This state of affairs diminishes normal cell function by interfering with internal cell signalling.
One of the conclusions seemed to be that if there is insufficient glutathione (GSH) available in the cell, the level of free radicals will increase. An imbalance represented by high levels of free radicals results in oxidative stress and cellular inflammation. This state of affairs diminishes normal cell function by interfering with internal cell signalling.