 This is a topic that is somewhat dear to my heart. My sister was diagnosed with Fibromyalgia a couple of decades ago. And her life has been miserable for much of that time.
This is a topic that is somewhat dear to my heart. My sister was diagnosed with Fibromyalgia a couple of decades ago. And her life has been miserable for much of that time.
Terminology
For clarification, ME refers to Myalgic Encephalomyelitis or Myalgic Encephalopathy, CFS refers to Chronic Fatigue Syndrome, and FMS refers to Fibromyalgia Syndrome (more commonly just Fibromyalgia).
ME/CFS
Chronic Fatigue Syndrome is a term that has been in use for quite some time. A name less recognized in Canada but moving into more common use is myalgic encephalomyelitis (ME). This lengthy name can be easily broken down into its parts, where “myalgic” refers to muscle pain; “encephalo” refers to the brain; “myel” refers to the spinal cord; and “itis” refers to inflammation.
In 2001, Health Canada appointed an international panel of experts in this emerging field of medicine to establish a clinical working-case definition, diagnostic guidelines, and treatment procedures. The panel released a set of guidelines in 2003 and their choice of name to describe the condition was both “myalgic encephalomyelitis” and “chronic fatigue syndrome” – with acronyms shortening it down to a manageable size: ME/CFS.
It is estimated that more than 1 million people in the US population have ME/CFS – 422 per every 100,000 people. It is 4 times as common in women as in men (522 out of 100,000 women have it), and women suffer from ME/CFS in greater numbers than from breast cancer (26 per 100,000), HIV/AIDS (12 per 100,000), or lung cancer (33 per 100,000).
In Canada, Statistics Canada reported in 2005 that over 341,000 Canadians were diagnosed with ME/CFS.
~~ Source: medbroadcast.com
Refer also to a more recent definition from the U.S. Centres for Disease Control and Prevention. Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
FMS
FMS stands for Fibromyalgia Syndrome. With Fibromyalgia, pain with its devastating and demoralizing effects remains a challenging problem for both patients and care givers. Fibromyalgia is one of the most common diseases affecting the muscles manifested with pain, stiffness, and tenderness of the muscles, tendons, and joints. The painful tissues involved are not accompanied by tissue inflammation. Therefore, despite potentially disabling body pain; patients with fibromyalgia do not develop tissue damage or deformity. The pain of fibromyalgia is generally widespread, involving both sides of the body. Pain usually affects the neck, buttocks, shoulders, arms, the upper back, and the chest. “Tender points” are localized tender areas of the body that can bring on widespread pain and muscle spasm when touched.
FMS typically presents in young or middle-aged females as persistent widespread pain, stiffness, fatigue, disrupted unrefreshing sleep, and cognitive difficulties, often accompanied by multiple other unexplained symptoms, anxiety and/or depression, and functional impairment of daily living activities. There is an overall 6% to 15% prevalence rate in the United States with a five times greater incidence among women than men.
~~ Source: Oman Medical Journal, published May 2012.
ROS
ROS stands for Reactive Oxygen Species, otherwise known as “free radicals.” Oxidative Stress is a condition in which the level of free radicals exceeds the antioxidant capacity of the body – there’s not enough antioxidants to neutralize the radicals and maintain a balance. (Refer to the article Get Rid of the Radicals.) As most people know, radicals are bad for your health. Prolonged periods of oxidative stress lead to disease and disfunction.
Both ME/CFS and FMS exhibit oxidative stress as a common characteristic.
According to a study published in 2014, “Many studies involving peripheral blood measurements have demonstrated significant abnormalities related to increased O&NS [oxidative stress and nitrosative stress] in many patients with ME/CFS.” (Ref. 1)
According to a study published in 2015, “FMS patients have higher oxidative stress index and lower total nitrite levels than healthy controls. In particular, patients with FMS demonstrated higher serum prolidase activity, total oxidative status, and oxidative stress index than healthy controls, and serum prolidase activity positively correlated with pain and fatigue scores.” (Ref. 2)
My Sister’s Story
My sister had been living with a diagnosis of Fibromyalgia for at least a couple of decades. Several days a week she would have difficulty getting out of bed in the morning. Either not enough energy or too much pain or both. And when she did get up and going, everything she did caused pain and drained her energy. This was no way to live. I’m sure I have just glossed over the situation since I have not experienced what she goes through on a daily basis. I could not do justice to her challenges.
A few years ago I became aware of a nutritional supplement that increased the body’s intracellular glutathione levels. And I saw a list of conditions associated with low glutathione. When I saw Fibromyalgia on the list, my attention perked up.
My Mom and my sister live separately but in the same house. And they live about a five hour drive away from where I live. One weekend when I went to visit, I told my sister about the supplement and urged her to try it. I would be her supplier. She agreed – but I think it was because I was her brother and not because she thought it would make a difference.
After I went home I would call my Mom every couple of weeks to see how she was doing. During those calls I would ask about my sister.
“How’s Sue doing?”
My Mom would answer, “Oh, she’s doing alright.”
A few weeks later, “How’s Sue doing?”
“She’s doing alright.”
“How’s Sue doing?”
“She’s doing alright.”
I was starting to get frustrated. This supplement was supposed to help her.
About 8-10 weeks after she started on the supplements, “How’s Sue doing?”
“Oh, she’s had a particularly bad day today.”
I was thinking, “Damn, the stuff was supposed to help.” But before I could say anything, my Mom went on, “You know those pills you gave her?”
“Yeeesss.” I said somewhat hesitantly. I feared she was going to tell me she thought the supplement had caused problems.
Mom said, “Well, her energy levels are up so much and her pain levels are down so much that she’s doing stuff she hasn’t done in 20 years and her muscles are complaining.”
I was shocked. But before I could even think of a response, my mother starts crying and says, “Thank you for giving your sister her life back.”
All I did was suggest that she take some supplements, based on some science research I had done. But I must admit that it felt pretty good.
We later determined that she needed to take more than the standard dose recommended by the manufacturer to see adequate benefits. Things will never get back to the way they were when she was twenty. But they are an order of magnitude better than what they used to be.
Summary
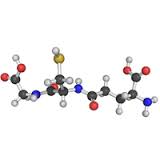
Both ME/CFS and FMS exhibit high levels of oxidative stress (high levels of damaging free radicals). The high level of oxidative stress correlates to high pain and fatigue scores. Glutathione is the body’s master antioxidant. It is produced by the body inside each living cell. Researchers use the level of glutathione as the primary indicator of the level of oxidative stress – the lower the glutathione level the higher the oxidative stress.
Experience shows that increasing intracellular glutathione reduces oxidative stress levels, which leads to a reduction of pain and fatigue. This approach is not a cure; but it may be an effective way to improve the quality of life of those dealing with these conditions.
References:
Reference 1: Gerwyn Morris and Michael Maes, Oxidative and Nitrosative Stress and Immune-Inflammatory Pathways in Patients with Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS), Current Neuropharmacology, 2014 Mar; 12(2): 168–185. Mar. doi: 10.2174/1570159X11666131120224653
Reference 2: Theoharis C. Theoharides, Irene Tsilioni, Lauren Arbetman, Smaro Panagiotidou, Julia M. Stewart, Rae M. Gleason, and Irwin J. Russell, Fibromyalgia Syndrome in Need of Effective Treatments, The Journal of Pharmacology and Experimental Therapeutics, 2015 Nov; 355(2): 255–263. Published online 2015 Nov. doi: 10.1124/jpet.115.227298
#Fibromyalgia #ChronicFatigue #ME/CFS #glutathione
Another Great Article John.
Looking forward to see many more!
Thank you, Stan. I really appreciate your feedback.
~~ John